Being the third most common cancer worldwide and responsible for a significant number of cancer-related deaths, colorectal cancer is the cancer which affects the colon and rectum part of the digestive tract. While many factors contribute to the development of colorectal cancer, genetics is increasingly recognized as an important risk factor. In this article, we will discuss the role of genetic testing in identifying the risk for colorectal cancer
While the majority of colorectal cancer cases are sporadic (i.e., not caused by an inherited genetic mutation), a small percentage of cases are caused by inherited genetic mutations that increase the risk of developing colorectal cancer. In this context, genetic testing can play an important role in identifying individuals who may be at increased risk of developing colorectal cancer and who may benefit from earlier and more frequent screening.
As one of the best colorectal cancer surgeons in Surat, Dr. Dhaval Mangukiya understands the importance of genetic testing in identifying patients at risk for the disease. Genetic testing is a process that examines a person’s DNA for specific changes or mutations that may increase their risk of developing cancer. There are several types of genetic testing available for colorectal cancer, including single-gene testing, multi-gene panel testing, and whole exome sequencing.
The two main types of inherited colorectal cancer syndromes are familial adenomatous polyposis (FAP) and Lynch syndrome, also known as hereditary non-polyposis colorectal cancer (HNPCC). FAP is caused by mutations in the APC gene and is characterized by the development of hundreds to thousands of polyps in the colon and rectum, which can progress to cancer if left untreated. Lynch syndrome is caused by mutations in one of several DNA mismatch repair genes and is characterized by an increased risk of developing colorectal cancer as well as other types of cancer, including endometrial, ovarian, stomach, pancreatic, and urinary tract cancers.
Genetic testing for FAP and Lynch syndrome involves analysing a person’s DNA for mutations in the APC gene or DNA mismatch repair genes, respectively. This testing can be done using a blood or saliva sample and can detect mutations with high accuracy. If a mutation is identified, family members can also be tested to determine if they have inherited the same mutation and are therefore at increased risk of developing colorectal cancer.
In addition to FAP and Lynch syndrome, there are several other inherited genetic mutations that have been associated with an increased risk of developing colorectal cancer. These include mutations in the MUTYH, BMPR1A, and SMAD4 genes, among others.
As the best colon cancer surgeon in Surat, Dr. Mangukiya emphasizes the importance of genetic testing for individuals with a family history of colorectal cancer. “If you have a first-degree relative, such as a parent or sibling, who has been diagnosed with colorectal cancer, you should consider genetic testing,” he says. “Even if you don’t have a family history, if you are concerned about your risk for the disease, talk to your doctor about whether genetic testing may be appropriate for you.”
In addition to identifying individuals at increased risk for colorectal cancer, genetic testing can also help guide treatment decisions for patients with the disease. “If we know that a patient’s tumor has a specific genetic mutation, we can tailor their treatment to that mutation,” says Dr. Mangukiya, who is also one of the best gastro surgeons in Surat. “This can lead to more effective treatment and better outcomes for the patient.”
One of the main benefits of genetic testing for colorectal cancer risk is the ability to identify individuals who may benefit from earlier and more frequent screening. For example, individuals with FAP or Lynch syndrome are typically recommended to undergo regular colonoscopies starting at a younger age (e.g., age 20–25) and at more frequent intervals (e.g., every 1–2 years) than individuals at average risk. This increased screening can help to detect polyps and early-stage cancers at a more treatable stage, ultimately leading to better outcomes.
In addition, genetic testing can help to inform decisions about preventive measures. For example, individuals with FAP are typically recommended to undergo prophylactic colectomy (i.e., surgical removal of the colon) to prevent the development of cancer. While this is a major surgical procedure, it can significantly reduce the risk of developing colorectal cancer in individuals with FAP.
Genetic testing for colorectal cancer risk can also have important implications for family members. If a mutation is identified in an individual, their first-degree relatives (i.e., parents, siblings, and children) have a 50% chance of inheriting the same mutation and being at increased risk of developing colorectal cancer. Family members can undergo genetic testing to determine if they have inherited the mutation, and if so, they can also undergo earlier and more frequent screening to reduce their risk of developing colorectal cancer.
However, it is important to note that genetic testing for colorectal cancer risk is not appropriate for everyone. It is typically recommended by a colorectal cancer specialist for individuals with a family history of colorectal cancer with the help of the guidance of a colorectal surgeon.
FAQ’S
What are the genetic risk factors of colorectal cancer?
Colorectal cancer (CRC) is a complex disease with multiple genetic and environmental risk factors. Some of the most common genetic risk factors for CRC include:
- Inherited mutations in certain genes: Mutations in genes such as APC, MLH1, MSH2, MSH6, PMS2, and EPCAM can increase the risk of developing CRC.
- Family history of CRC: Having a first-degree relative (parent, sibling, or child) with CRC increases a person’s risk of developing the disease.
- Age: The risk of CRC increases as people get older.
- Inflammatory bowel disease (IBD): Long-standing inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease increase the risk of developing CRC.
- Personal history of certain types of polyps: Certain types of polyps, such as adenomatous polyps, can increase the risk of CRC.
- Lifestyle factors: Factors such as a diet high in red meat and processed foods, physical inactivity, smoking, and heavy alcohol consumption have been associated with an increased risk of CRC.
It’s important to note that while having one or more of these genetic risk factors increases a person’s likelihood of developing CRC, it doesn’t necessarily mean that they will develop the disease. Regular screening and early detection can help to prevent and treat CRC as explained by Dr. Dhaval Mangukiya, one of the best colon cancer specialists in Surat.
What does testing to determine the risk of colorectal cancer include?
There are different types of tests that can help determine a person’s risk of colorectal cancer (CRC). Some of the most common ones are as follows:
- Family history assessment: This involves gathering information about a person’s family history of CRC and other related cancers. A healthcare provider may ask questions about the number of relatives affected, their ages at diagnosis, and any other relevant medical information.
- Genetic testing: This involves analyzing a person’s DNA for inherited mutations that are known to increase the risk of CRC, such as mutations in the APC, MLH1, MSH2, MSH6, PMS2, and EPCAM genes.
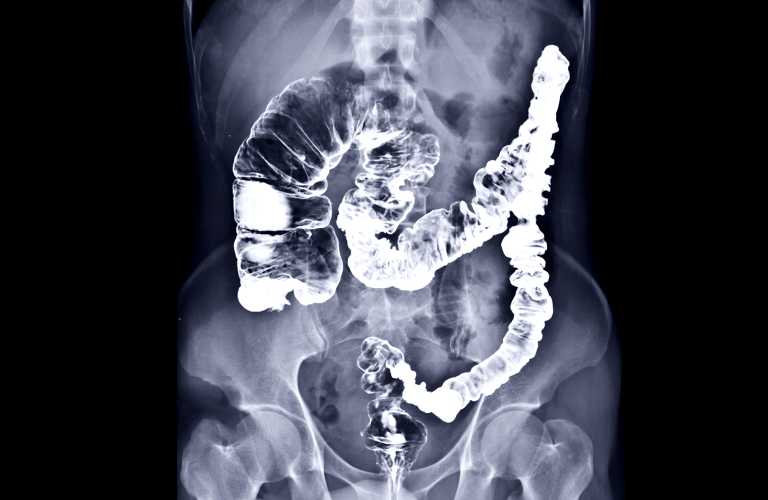
- Colonoscopy: This is a procedure that uses a flexible, lighted tube with a camera to examine the inside of the colon and rectum. Colonoscopy can detect precancerous polyps and early-stage CRC, which can be removed before they become cancerous.
- Fecal occult blood test (FOBT): This is a non-invasive test that checks for the presence of blood in the stool, which can be a sign of CRC. FOBT can be done at home and mailed to a lab for analysis.
- Stool DNA test: This is a newer type of non-invasive test that checks for DNA changes in the stool that may indicate the presence of CRC or precancerous polyps.
It’s important to talk to a colon cancer specialist about the appropriate testing based on an individual’s age, personal and family medical history, and other risk factors.
How are genetic tests for cancer risk performed?
Genetic testing for cancer risk involves analyzing a person’s DNA to look for mutations or changes in specific genes that are known to increase the risk of developing cancer. Here is an overview of how genetic tests for cancer risk are performed:
- Consultation: The first step is to meet with a healthcare provider or genetic counselor to discuss the benefits, risks, and limitations of genetic testing. They will review a person’s medical and family history to determine if genetic testing is appropriate.
- Sample collection: Genetic testing requires a sample of a person’s DNA. This can be obtained from a blood sample, saliva sample, or tissue biopsy.
- Laboratory analysis: The DNA sample is sent to a laboratory that specializes in genetic testing. The lab will use specialized equipment and techniques to analyze the DNA for mutations in specific genes associated with cancer risk.
- Test results: Once the laboratory analysis is complete, the healthcare provider or genetic counselor will review the results with the person. If a genetic mutation is found, they will discuss the implications of the result and recommend appropriate medical management or screening.
Genetic testing can be complex and may have emotional and psychological implications. Therefore, it’s important to consult the best gastro surgeon in Surat to understand the potential benefits and risks before deciding to undergo genetic testing.